For several decades, both synthetic and natural materials have been explored for use as scaffolds in tissue engineering. Artificial extracellular matrices (aECMs) are an extension of biomaterials that were developed to provide a model environment for tissue cells in-vitro that mimic the native surroundings of the target tissue in vivo.
Over the years, the use of aECMs has attained an excellent reputation in the field of tissue engineering due to their exceptional mechanical properties, processability and low cost. Artificial ECMs are generally classified as either a natural polymer-based, synthetic polymer-based, or hybrid material, and they differ based on their component materials.
Design of artificial ECMs is very important in tissue engineering, because artificial ECMs regulate many cellular behaviors, including proliferation and growth, survival, change of cell shape, migration, and differentiation. Also, artificial ECMs have multiple functions, such as serving as an adhesive substrate, provision of structure, presentation and storage of growth factors, and detection of signals.
Novel designs of aECMs from synthetic materials are a possible alternative due to their minimal risk of pathogen transmission, lack of immune response and the ability for greater control over material properties and tissue responses. The type of target tissue, accessibility and the biological or therapeutic application of the study are all a few factors to take into consideration when choosing between the various biomaterials available.
This physical network provides not only structure and support, but is also the biological information that plays an important role in guiding development, maintaining homeostasis and directing regeneration of cells in a tissue-specific manner.
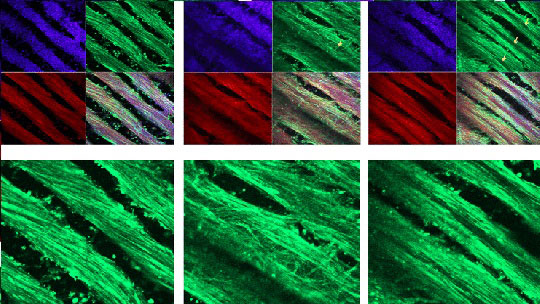
Most ECM in vivo has the collagen fibril as a central building block, and consequently collagen, especially collagen type I, is most commonly used in constructing an aECM. The basis of aECM is in the majority of cases collagen, just as it is the basis of ECM in the body.
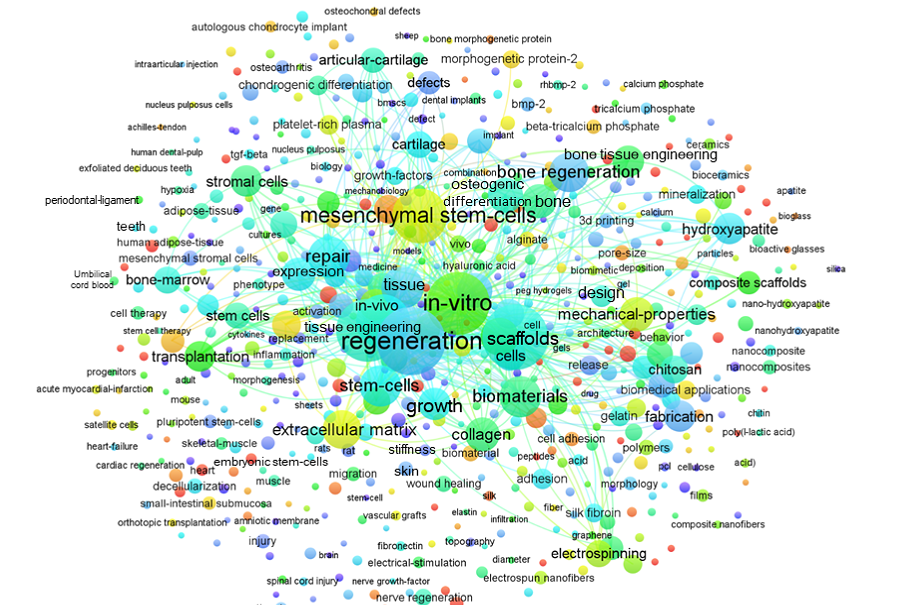
The emergence of biomaterials for regeneration has increased collaborations between engineers, scientist and clinicians to design materials that address the specific criteria for repairing this type of injury. Tissue damage to skin, bone, liver, lung, heart and the vascular system are among a few targets that also utilize aECM strategies to study potential treatment and repair. With increasing cases of organ shortages and donor scarcity within the last three decades, the research focus in the field of regenerative medicine and tissue engineering continues to advance toward a potential therapeutic for various types of tissue damage.
3D scaffolds and matrices arranged to mimic the native micro-environment and biological components within the body are continuing to evolve and advance over time. However, there are still limitations and challenges that need to be settled before they can be considered suitable for clinical application. There are a number of hurdles that raise concerns, such as ensuring that materials are harmless to the host and that they support the composition and function of the cells, immune complications, and spatial constraints.